New approach to call handling is saving lives, study finds
A call-handling model introduced by the Scottish Ambulance Service to enhance its response to patients with life-threatening conditions has improved survival rates, new research has revealed.
/filters:format(webp)/filters:no_upscale()/prod01/cdn/media/stirling/news/news-centre/2019/february/ambulance-1920X689.jpg)
A call-handling model introduced by the Scottish Ambulance Service to enhance its response to patients with life-threatening conditions has improved survival rates, new research has revealed.
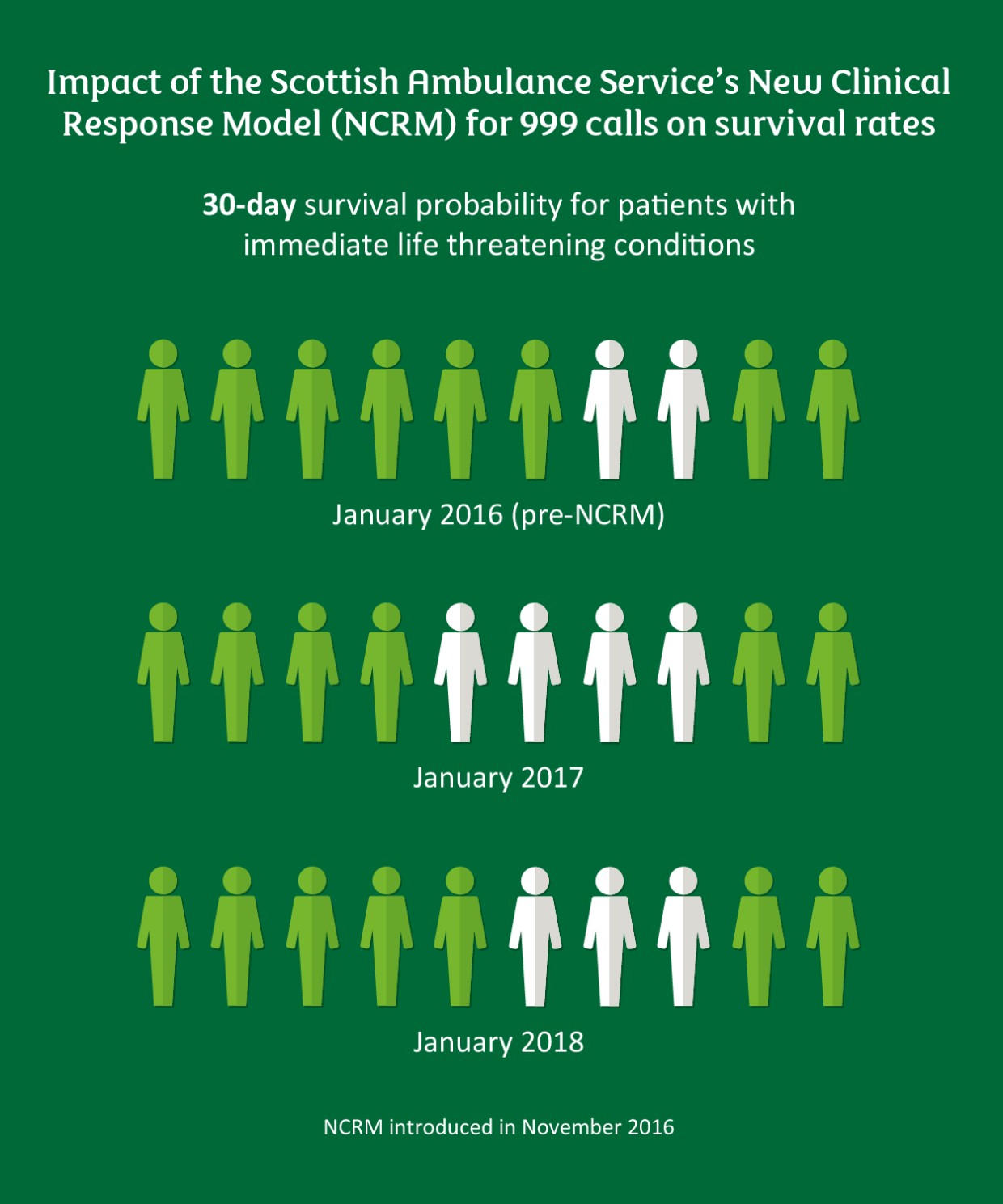
The University of Stirling study found that the New Clinical Response Model (NCRM) for 999 calls – introduced in November 2016 – improved 30-day survival in patients with immediate life threatening (ILT) conditions. Comparing January data from 2016, 2017 and 2018, the team found that survival increased by 20 per cent in January 2017 and 10 per cent in January 2018.
In January 2016, before the new model was introduced, two in 10 patients with ILT conditions were likely to survive. Under the new model, that increased to four in 10 in January 2017 and three in 10 in January 2018.
The scientists said the new model improved accuracy in identifying those with ILT conditions and resulted in stable response times for those in that category. However, the prioritisation of the most critical patients has led to longer response times for those in less serious conditions, they added.
Professor Jayne Donaldson, Dean of the Faculty of Health Sciences and Sport at Stirling, led the research, which also involved Glasgow Caledonian University.
Professor Donaldson said: “Our study analysed data from January 2016 – before the NCRM was introduced – and the same period in 2017 and 2018, after it was implemented.
“We found that the new model can accurately identify patients who have the greatest need for ambulance services. While the identification and triage of patients takes time for the call handler and dispatching system, the NCRM can get an ambulance crew to patients who need them most.
“Ultimately, this approach has improved the survival of those with immediate life threatening conditions.”
/filters:format(webp)/filters:no_upscale()/prod01/cdn/media/stirling/news/news-centre/2019/february/JayneDonaldson-700X600.jpg)
Dean of the Faculty of Health Sciences and Sport
These conclusions are reached in the context of analysing aggregated data over three fairly short time-periods. Further research over a longer timeframe, with longitudinal data on individual cases, would improve the evidence base for NCRM.
The Scottish Ambulance Service (SAS) responds to around 1.8 million calls per year, including 700,000 emergency and unscheduled incidents. Of these responses, more than 500,000 are received via 999 calls.
Prior to the introduction of NCRM, the SAS used a model focused on a response time of eight minutes for all incidents. However, this approach led to the dispatching of resources with no awareness of the patient’s clinical need; dispatching multiple resources in the hope that one would hit the target; and mismatching the type of resource to the need of the patient.
The new model was introduced with the aim to save more lives – by improving the accuracy in identifying patients with immediately life-threatening conditions, such as cardiac arrest, and ensuring the first resource dispatched is the most appropriate, based on patients’ clinical needs.
NCRM is a colour-coded system, which categorises 999 calls in terms of priority. Cases are coded purple, red, amber, yellow and green. Patients with ILT conditions are categorised purple – the most urgent cases, where patients’ risk of cardiac arrest is above 10 per cent.
The researchers conducted a quantitative analysis on the response to 999 calls from a pre-NCRM timeframe (January 2016) and two post-implementation periods (January 2017 and January 2018). In addition, they analysed emergency department and mortality data for each period.
The researchers noted a 20 per cent increase in 30-day survival for all purple-coded patients, comparing January 2016 and 2017, and 10 per cent, comparing January 2016 and 2018.
In all other categories, survival remained unchanged over the three time-periods.
Comparing January 2016 and 2018, the response time for purple-coded incidents remained relatively stable; however, it was slower in all other categories. Significantly, in January 2018, the demand for SAS services was notably higher than in January 2016 and 2017 – responding to more than 4,000 (nine per cent) additional incidents.
Professor Donaldson said: “Those with lower acuity needs are responded to, but in a longer time-period – as is expected when using a priority-based system. However, there is no apparent negative impact on survival.
“These conclusions are reached in the context of analysing aggregated data over three fairly short time-periods. Further research over a longer timeframe, with longitudinal data on individual cases, would improve the evidence base for NCRM.”
Professor Donaldson also called for further research on the impact of the new model to consider health and social care outcomes other than survival, such as patient experience, readmission rates and quality of life.
The research – funded by the Scottish Ambulance Service – also involved Dr Kathleen Stoddart, Dr Tony Robertson, Dr Carol Bugge and Dr Federico Andreis, all from the University of Stirling, and Dr Julie Cowie, of Glasgow Caledonian University.
